Delayed Clinically Significant Portal Hypertension after Total Pancreatectomy-Islet Auto-Transplantation
Nicholas Lim 1,*![]() , Gregory Beilman 2
, Gregory Beilman 2![]() , Timothy Pruett 2
, Timothy Pruett 2![]()
- Department of Medicine, University of Minnesota, Minneapolis, Minnesota, USA
- Department of Surgery, University of Minnesota, Minneapolis, Minnesota, USA
* Correspondence: Nicholas Lim![]()
Received: March 21, 2018 | Accepted: June 7, 2018 | Published: June 12, 2018
OBM Transplantation 2018, Volume 2, Issue 2 doi:10.21926/obm.transplant.1802011
Academic Editors: Kenneth Brayman and Pål Dag Line
Special Issue: Current Advancement of Islet Cell Transplantation in the Treatment of Diabetes Mellitus
Recommended citation: Lim N, Beilman G, Pruett T. Delayed Clinically Significant Portal Hypertension after Total Pancreatectomy-Islet Auto-Transplantation. OBM Transplantation 2018;2(2):011; doi:10.21926/obm.transplant.1802011.
© 2018 by the authors. This is an open access article distributed under the conditions of the Creative Commons by Attribution License, which permits unrestricted use, distribution, and reproduction in any medium or format, provided the original work is correctly cited.
Abstract
Portal hypertension often occurs transiently with injection of islet cells into the portal system during total pancreatectomy-islet autotransplantation (TPIAT). We describe a TPIAT patient with non-cirrhotic portal hypertension (NCPH) two years after surgery initially identified with esophageal varices on upper endoscopy. The underlying mechanism for the development of NCPH after TPIAT is unclear but infectious and immune-related pathways have been proposed. Management of NCPH is primarily treatment of complications such as esophageal varices and ascites. The long-term prognosis of NCPH in TPIAT remains unclear.
Keywords
Total pancreatectomy-islet autotransplantation; chronic pancreatitis; portal hypertension; liver function; splenectomy
1. Introduction
Total pancreatectomy-islet autotransplantation (TPIAT) was first performed in 1978 and has proven to be a life-changing surgery for thousands of patients with chronic pancreatitis [1]. The surgery involves injection of a preparation of the patient’s islet cells into the portal system resulting in a significant but transient elevation in portal pressures. We report a case of a patient with clinically significant portal hypertension identified two years following TPIAT for idiopathic chronic pancreatitis.
2. Case
A 35-year-old male underwent TPIAT at our institution for idiopathic chronic pancreatitis. Evaluation for etiologies of chronic pancreatitis including genetic testing had all returned negative. The patient had initially presented with a 6-year history of intermittent right-sided abdominal and flank pain. After seeing several specialists from different disciplines, he ultimately underwent endoscopic ultrasound which was consistent with chronic pancreatitis. Of note, upper endoscopy performed at the same time showed a normal esophagus and normal stomach. Magnetic resonance imaging (MRI) abdomen with secretin confirmed parenchymal changes consistent with chronic pancreatitis but a normal secretin response.
During his pre-TPIAT evaluation, the patient was found to have mildly abnormal liver function tests and was referred to hepatology clinic. Serological and genetic testing were negative for viral hepatitis, celiac disease, hemochromatosis, Wilson’s disease, autoimmune hepatitis and alpha-1 anti-trypsin deficiency. Imaging and blood testing showed no evidence of cirrhosis or portal hypertension. The patient’s abnormal liver function tests were attributed to mild non-alcoholic fatty liver disease and were not determined to be a contraindication in proceeding with TPIAT. By this time, the patient was taking increasing doses of chronic narcotic pain medication and regular anti-emetics for control of his pain and nausea symptoms related to chronic pancreatitis.
The patient underwent TPIAT two years ago without complication. Mild peri-pancreatic adhesions were noted at the time of total pancreatectomy and cholecystectomy, splenectomy, duodenectomy, appendectomy with construction of a roux-en-Y jejunojejunostomy were performed per center protocol. The excised pancreas was infused with alpha-1 anti-trypsin solution and sent to the islet team for preparation. 432,400 islets (3638 islet equivalents/kilogram) were infused via a 20ml tissue volume into the middle colic vein. 2800 units of heparin were infused before and with delivery of islets. Pre-infusion portal pressure was 9cm/H20 and post-infusion portal pressure was 27cm/H20. Final post-rinse portal pressure measured 31cm/H20. The patient made a good recovery in the post-operative period and was discharged home after ten days.
The patient was weaned off narcotic pain medication and anti-emetics over several months after TPIAT. He returned to work part-time soon after, eventually increasing his hours to full-time within twelve months of surgery.
Twenty-two months after TPIAT, the patient presented to his primary care physician with acute onset, severe, burning upper abdominal pain with associated hematemesis after an upper respiratory tract infection. The patient was admitted to hospital for IV fluids and IV proton pump-inhibitor therapy. Computerized tomography (CT) abdomen and pelvis with IV contrast showed a hyperemic proximal jejunum. The patient’s symptoms improved quickly and he was discharged from hospital with a plan to undergo outpatient upper endoscopy later that week.
The patient underwent upper endoscopy without difficulty. Erosions in the proximal jejunum corresponded to the abnormal area seen on CT earlier in the week. Mild erythema was noted in the stomach and biopsied to rule out h.pylori infection. Unexpectedly, small esophageal varices were seen in the lower esophagus (Figure 1). Gastric varices and portal hypertensive gastropathy were not observed.
Figure 1 Endoscopic image of small esophageal varices (yellow arrows) in the lower third of the esophagus.
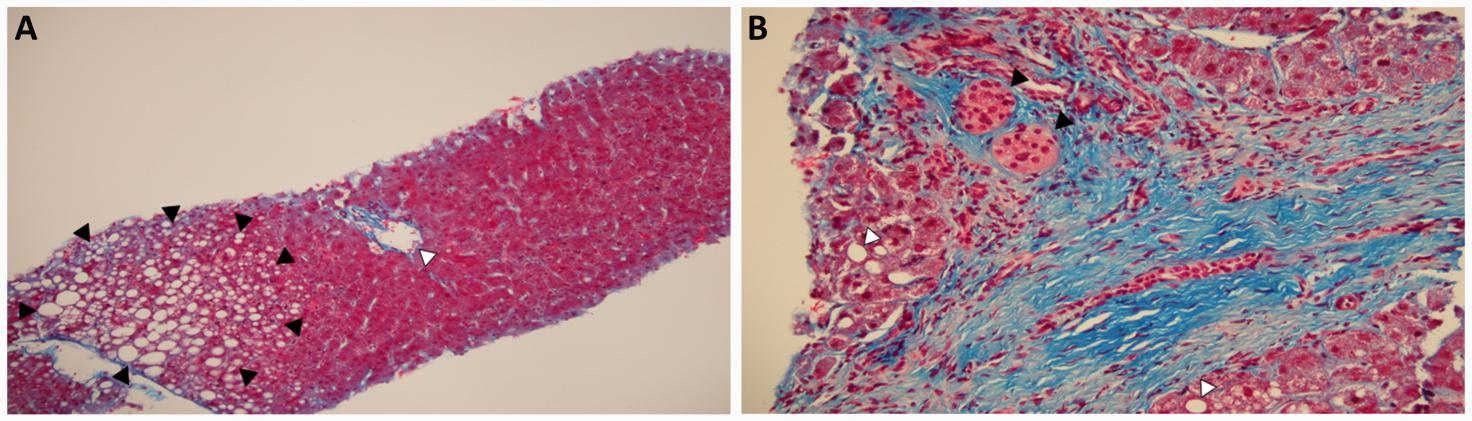
The patient was then referred for transjugular liver biopsy with portal pressure measurements. Porto-systemic gradient measured 12mmHg. Liver biopsy showed normal liver parenchyma, a small amount of hepatic steatosis and scarce islets in the portal tracts (Figure 2). Trichrome stain showed no evidence of hepatic fibrosis or cirrhosis. CT angiogram of the abdomen was obtained and showed patent hepatic vasculature and no evidence of portal vein thrombosis or ascites. Varices were seen in the esophagus and around the gastro-jejunal anastomosis (Figure 3).
Figure 2 Liver biopsy: (A) Low power view of normal hepatic parenchyma with normal portal tract (white arrow) and a small amount of macrovesicular hepatic steatosis (black arrows). No evidence of bridging fibrosis, nodule formation or cirrhosis. Trichrome stain; (B) High power view of two clusters of engrafted islet cells in the portal tract (black arrows) with minimal macrovesicular steatosis in the hepatic parenchyma (white arrows). Trichrome stain.
Figure 3 CT angiogram of abdomen: (A) Coronal view showing normal portal vasculature including patent portal vein (yellow arrow) and normal hepatic contour; (B) Axial view showing gastro-jejunal varices (yellow arrows) at gastro-jejunal anastomosis.
The patient has since been seen in hepatology clinic. He continues to do well post-TPIAT from the point of view of abdominal pain and has no symptoms of ascites or hepatic encephalopathy. He is planned to undergo repeat upper endoscopy in one year to evaluate for progression or regression of esophageal varices.
3. Discussion
This is the first case of persistent and clinically significant portal hypertension following TPIAT to be reported in the literature. Patients undergoing TPIAT typically experience rises in portal pressures intra-operatively at the time of islet cell injection but this is the first documented case of portal hypertension to be described two years after transplantation. This finding is particularly unexpected with TPIAT in the context of a concurrent splenectomy, an operation performed to manage portal hypertension.
The patient’s liver biopsy showed no evidence of cirrhosis and minimal hepatic steatosis. In addition, evaluation prior to TPIAT showed no evidence of cirrhosis or portal hypertension, consistent with a diagnosis of idiopathic non-cirrhotic portal hypertension (NCPH).
NCPH has a high prevalence in India with an estimated incidence of 23% but is relatively rare in the Western world. Schistosomiasis is the most common cause of NCPH worldwide but in the West, it is associated with exposure to various medications e.g. azathioprine and toxins e.g. arsenic [2,3].
The underlying pathophysiologic mechanism for NCPH remains unclear although infectious and immune-mediated processes have been implicated. Animal studies have demonstrated NCPH after injection of Escherichia coli into the portal vein. It is thought that septic microemboli may lead to obstruction of small portal veins to cause the development of portal hypertension [4]. Animal studies have also demonstrated the development of portal hypertension in rabbit models following injection of splenic extract into the portal system with associated elevation in inflammatory markers and cytokines suggestive of an immune-related process [5]. An immune-related mechanism seems more likely in our patient given his uncomplicated post-operative course although the islet cells transplanted were autologous.
The management of non-cirrhotic portal hypertension typically focuses on complications of portal hypertension. Our patient was diagnosed incidentally but a significant proportion of patients with non-cirrhotic portal hypertension present with acute variceal hemorrhage. Endoscopic band ligation and non-selective beta-blockers are the mainstay of therapy in this population based on evidence-based practice guidelines for patients with cirrhosis. Shunt surgery and transjugular intrahepatic porto-systemic shunt (TIPS) have both been reported for bleeding refractory to endoscopic therapy [2].
The long-term survival for patients with non-cirrhotic portal hypertension is unclear. Early reports described similar long-term survival to patients with cirrhosis but were based on data gathered prior to advances in liver transplantation and endoscopic therapy [6,7]. More recently, two studies have described worse long-term survival compared to patients with cirrhosis although most deaths were related to associated malignancy and not liver-related complications [8,9]. Our patient’s long-term survival related to the development of non-cirrhotic portal hypertension after TPIAT therefore remains unclear.
In summary, we describe the first case of persistent portal hypertension in a patient following TPIAT. The clinical course of NCPH after TPIAT is unclear but prospective management should focus on the prevention of variceal hemorrhage. Future research efforts should be focused on determining the pathophysiology and long-term survival of this condition.
Acknowledgments
We would like to acknowledge Dr Dale Snover for providing pathology images and Dr Tina Sanghvi for providing radiology images.
Author Contributions
Nicholas Lim- initial draft of manuscript, revision of manuscript; Gregory Beilman- revision of manuscript; Timothy Pruett- critical revision of manuscript.
Competing Interests
The authors have declared that no competing interests exist.
References
- Sutherland DE, Matas AJ, Najarian JS. Pancreatic islet cell transplantation. Surg Clin North Am. 1978; 58: 365-382. [CrossRef]
- Schouten JN, Garcia-Pagan JC, Valla DC, Janssen HL. Idiopathic noncirrhotic portal hypertension. Hepatology. 2011; 54: 1071-1081. [CrossRef]
- Sherlock S. Noncirrhotic extrahepatic and intrahepatic portal hypertension. Semin Liver Dis. 1982; 2: 202-210. [CrossRef]
- Omanwar S, Rizvi MR, Kathayat R, Sharma BK, Pandey GK, Alam MA, et al. A rabbit model of non-cirrhotic portal hypertension by repeated injections of E.coli through indwelling cannulation of the gastrosplenic vein. Hepatobiliary Pancreat Dis Int. 2004; 3: 417-422.
- Kathayat R, Pandey GK, Malhotra V, Omanwar S, Sharma BK, Sarin SK. Rabbit model of non-cirrhotic portal fibrosis with repeated immunosensitization by rabbit splenic extract. J Gastroenterol Hepatol. 2002; 17: 1312-1316. [CrossRef]
- Kingham JG, Levison DA, Stansfeld AG, Dawson AM. Non-cirrhotic intrahepatic portal hypertension: A long term follow-up study. Q J Med. 1981; 50: 259-268.
- Sarin SK, Kapoor D. Non-cirrhotic portal fibrosis: current concepts and management. J Gastroenterol Hepatol. 2002; 17: 526-534. [CrossRef]
- Schouten JN, Nevens F, Hansen B, Laleman W, van den Born M, Komuta M, et al. Idiopathic noncirrhotic portal hypertension is associated with poor survival: results of a long-term cohort study. Aliment Pharmacol Ther. 2012; 35: 1424-1433. [CrossRef]
- Gioia S, Nardelli S, Pasquale C, Pentassuglio I, Nicoletti V, Aprile F, et al. Natural history of patients with non cirrhotic portal hypertension: Comparison with patients with compensated cirrhosis. Dig Liver Dis. 2018. DOI: 10.1016/j.dld.2018.01.132. [CrossRef]