Role of Automated Insulin Delivery (Artificial Pancreas) in Islet Transplantation: An In Silico Assessment
Dayu Lv ![]() , Jose Garcia-Tirado
, Jose Garcia-Tirado ![]() , Chiara Fabris *
, Chiara Fabris * ![]()
- Center for Diabetes Technology, University of Virginia, Charlottesville, VA, USA
* Correspondence: Chiara Fabris![]()
Received: May 17, 2018 | Accepted: August 30, 2018 | Published: September 13, 2018
OBM Transplantation 2018, Volume 2, Issue 3 doi:10.21926/obm.transplant.1803019
Academic Editor: Kåre I. Birkeland
Special Issue: Current Advancement of Islet Cell Transplantation in the Treatment of Diabetes Mellitus
Recommended citation: Lv D, Garcia-Tirado J, Fabris C. Role of Automated Insulin Delivery (Artificial Pancreas) in Islet Transplantation: An In Silico Assessment. OBM Transplantation 2018;2(3):019; doi:10.21926/obm.transplant.1803019.
© 2018 by the authors. This is an open access article distributed under the conditions of the Creative Commons by Attribution License, which permits unrestricted use, distribution, and reproduction in any medium or format, provided the original work is correctly cited.
Abstract
Background: Human pancreatic islet transplantation is a minimally-invasive procedure that is gaining recognition for the treatment of type 1 diabetes (T1D). Selected patients with unstable T1D, hypoglycemia unawareness, history of severe hypoglycemia, and glycemic lability, not successfully stabilized with intensive insulin treatment, can be offered this alternative therapy that has been shown to provide long-term glycemic control with near-normalization of hemoglobin A1c in the absence of severe hypoglycemia. Today, downsides of pancreatic islet transplantation include the need for chronic recipient immunosuppression and the limited supply of pancreatic islets. In addition, attaining long-term insulin independence remains a challenge. In this context, stabilization of a patient’s metabolic system with islet transplantation that is augmented by automated insulin delivery (AID) technology could be of significant interest. In this manuscript, we want to frame and illustrate the problem of developing a combined bio-artificial system that includes an islet graft and mechanical AID.
Methods: Our discussion will propose modeling approaches potentially deployable in describing glucose homeostasis after islet transplantation and will be supported by a series of in silico studies simulating post-transplant glycemic patterns and the impact of AID control strategies. To run our analyses, we used the UVA/Padova T1D Simulator – a simulation platform accepted by FDA as a substitute to animal trials in the pre-clinical evaluation of insulin treatment strategies, appropriately modified to describe the glucose-insulin regulation system in transplanted individuals.
Results: The results presented here are a very preliminary in silico assessment of the benefits of combining islet transplantation and AID.
Conclusions: Further research, which relies on glucose and insulin data collected from transplanted patients, will be needed to optimize modeling and control strategies.
Keywords
Artificial pancreas; islet transplantation; modeling; UVA/Padova T1D simulator
1. Introduction
Type 1 diabetes (T1D) is a metabolic disorder characterized by the progressive immune-mediated destruction of insulin-producing β-cells in the islets of Langerhans [1]. In general, T1D results in absolute insulin deficiency, which requires affected individuals to rely on exogenous insulin to control exposure to hyperglycemia and reduce the progression of diabetes complications. Insulin therapy can include multiple daily insulin injections (MDI) or continuous subcutaneous insulin infusion (CSII), and can be aided by decision support systems designed to better inform insulin dosing. Although intensive insulin therapy has been widely shown to reduce the progression of micro- and macro-vascular diabetes complications, aggressive treatment with MDI or CSII is frequently associated with increased occurrence of hypoglycemic episodes, which can compromise hormonal defenses and warning symptoms for subsequent low blood glucose events [2,3]. Consequently, patients with T1D face a life-long optimization problem: to maintain a strict glycemic control without increasing the risk for hypoglycemia, which has been indeed identified as the major barrier to optimal diabetes management [4]. One possible solution to this problem is automated insulin delivery (AID) by means of closed-loop control algorithms, which is emerging as a viable treatment for T1D known as the “artificial pancreas” – a technology that now attracts considerable academic and industrial effort [5,6,7,8,9,10].
Individuals with unstable T1D, experiencing hypoglycemia unawareness, severe hypoglycemic episodes, and glycemic lability, who are not successfully stabilized by intensive insulin therapy, can be offered an alternative treatment – human pancreatic islet transplantation [11]. Islet transplantation is an effective β-cell replacement therapy that has the capacity to improve glycemic control, with near normalization of hemoglobin A1c (HbA1c) and reduction of glycemic variability, in the absence of severe hypoglycemic episodes [12,13,14,15]. The success rate of clinical islet transplantation has significantly improved with the advancement of techniques for islet isolation and preparation [16], and by optimizing post-transplant immunosuppression [12,17,18]. However, the need of lifelong anti-rejection immunotherapies and the limited supply of pancreas from deceased multi-organ donors represent relevant factors explaining why this therapy hasn’t been universally embraced for broad application [11].
While the primary success of islet transplantation has been to eliminate severe and recurrent hypoglycemia, the secondary benefit of attaining insulin independence has attracted patients but remains a challenge [16,17]. In the early Edmonton Protocol reports, ~11% of patients achieved sustained insulin independence, while the majority of individuals continued to need exogenous insulin administration [11]. Nevertheless, 73% of patients followed beyond 10 years in Edmonton demonstrated profound correction of glycemic control, with HbA1c levels corrected to <6.5%, positive C-peptide status, and ongoing protection from severe hypoglycemic events, with a degree of glycemic stabilization not possible by any technological means [11]. Thus, stabilization of a patient’s metabolic system with islet transplantation that is augmented by AID technology could be of significant interest.
The possibility of integrating islet transplantation with a post-transplant closed-loop insulin delivery that could supply any residual insulin needs can also have additional benefits. One can speculate that, in a context where insulin independence is not necessarily sought as an outcome of the transplantation procedure, AID could represent a significant breakthrough as it would reduce the glycemic stress the transplanted islets are exposed to, thus potentially extending the life of the graft. Further, this could lead to reduction of the number of transplanted islets needed to normalize glycemic control, with consequent increase of the islet supply and allowing patients to undergo less aggressive immunosuppressive regimens.
While these are speculations that have not been tested in animal or human studies, in this manuscript we attempt to shed light on the biomechanics of a combined bio-artificial system that includes an islet graft and mechanical AID, by conducting a series of in silico studies. We discuss open problems and possible strategies to model glucose homeostasis after islet transplantation resorting to a well-established computer simulation environment - the UVA/Padova T1D simulator, which has been in use for over 10 years and is accepted by the FDA as a substitute to animal trials in the pre-clinical evaluation of insulin treatment strategies [19,20,21,22,23]. To accommodate the problem in hand, we have used available literature [24] to modify the simulation environment and describe the glucose-insulin regulation system in transplanted individuals. Based on these modifications, we simulate and discuss the effect of control strategies to be implemented as part of an AID system deployable after islet transplantation.
2. Modeling the Glucose-Insulin Control System
In health, plasma glucose concentration is tightly regulated by a complex neuro-hormonal control system. Insulin is the primary regulator of glucose homeostasis, and the glucose and insulin sub-systems interact via feedback control loops [1]. In addition to insulin, glucagon plays a key role in the regulation of glucose levels, and acts as a counter-regulatory hormone to insulin [25]. Pancreatic islet alpha-cell glucagon secretion is critically dependent on pancreatic islet β-cell insulin secretion [26].
In T1D or advanced type 2 diabetes (T2D), the glucose-insulin-glucagon control system is degraded. In the absence of endogenous insulin secretion, circulating insulin levels depend only on the absorption and clearance of injected insulin, and fail to respond to raising or falling glucose concentration [27]. In addition, the lack of β-cell insulin decreases the alpha-cell inhibitory signal, which results in lack of increased alpha-cell glucagon secretion during hypoglycemia [27].
Several mathematical models have been developed in the last three decades to describe the glucose-insulin regulation system in T1D with the aim of assisting the optimization of diabetes control [1]. Models can be classified as minimal or maximal, depending on the degree of detail in the process description. Minimal models are parsimonious and describe the key components of system functionality; it is reasonable to assume that a good minimal model will not be a large-scale one: not every known substrate/hormone needs to be included because the macro-level response of the system would be relatively insensitive to many micro-level relationships, and many processes can be lumped together. In contrast, maximal models are comprehensive descriptions attempting to fully implement the body of knowledge about metabolic regulation into a generally large, nonlinear model of high order with a large number of parameters.
The oral minimal model method has been recently reviewed [28]. It consists of three models that allow the simultaneous estimation of insulin sensitivity (glucose minimal model), β-cell responsivity (C-peptide minimal model), and hepatic insulin extraction (insulin minimal model) from glucose, insulin, and C-peptide concentration time-series measured during a mixed-meal or an oral glucose tolerance test. The method was derived from the intravenous glucose tolerance test minimal model [29] and was validated by a series of triple tracer meal studies that have provided a rich database for its development.
A maximal model of the glucose-insulin regulation system has been presented in 2007 by Dalla Man and co-workers, with the purpose of providing a simulation tool capable of characterizing glucose control in the postprandial state [24]. The model describes the measured plasma glucose and insulin concentration time-series by means of glucose fluxes – rate of appearance, endogenous production, peripheral utilization, and renal extraction – and insulin fluxes – secretion (the model was developed to describe glucose control in health), hepatic extraction, and peripheral degradation. This model adapted to describe glucose metabolism in T1D, served as the foundation to the UVA/Padova T1D Simulator mentioned above. The governing equations of this model [20] will be here adapted to describe quantitatively glucose control and AID intervention after pancreatic islet transplantation. To do so, we need to take into consideration key elements of this type of T1D therapy, such as partially recovered endogenous insulin production and the impact of insulin signaling on the transplanted islet alpha-cell glucagon secretion. In addition, the graft site is likely to play a critical role in the in silico description of insulin secretion, e.g., on the time delay between secretion from the transplanted islets and appearance in the circulation.
On the assumption that islets are transplanted in the liver, insulin secretion can be modeled as a signal with amplitude depending on the number of transplanted islet equivalents that enters the hepatic circulation after a time delay, taking into account the location of the transplanted islets into the portal vein. Parameters governing first and second phase insulin secretion will be adapted from normal and T2D values estimated in [24] In addition, the control played by intraportal insulin concentration on endogenous glucose production needs to be introduced in the model, as described in [24]. In health, the amplitude of portal insulin action on the liver is described through a single parameter with value estimated by flux and concentration data [24]. Additional investigation and new data would be needed to estimate the optimal parameter value in transplanted patients using a Bayesian estimation strategy that extrapolates the information available for the parameter value distribution in health. Further, to describe the full glucose-insulin-glucagon control system, a model of islet alpha-cell glucagon secretion needs to be introduced to take into account the direct effect of endogenous insulin secretion on glucagon secretion, as well as any interactions with exogenous insulin [21].
3. The Automated Insulin Delivery System
AID technology, commonly known as the “artificial pancreas”, has become a focus of significant research and industrial development [30,31]. AID systems involve the pairing of continuous glucose monitoring (CGM) systems with CSII (insulin pump) via a closed-loop control algorithm which automatically adjusts insulin infusion in real-time[32], see Figure 1.

Figure 1 The closed-loop AID system for individuals with T1D. CHO stand for carbohydrates.
In the past decade, AID studies have advanced from short-term inpatient investigations using algorithm-driven manual control [33], to long-term clinical trials in free-living conditions using wearable wireless automated AID systems [34]. Reviews and collections of papers reflecting the progress of the AID field are published regularly [30,31,35,36], and report reduction of glucose variability, lower risk for hypoglycemia, reduced average glycaemia, and increased time in target ranges, particularly overnight. The first outpatient AID used a laptop-based system at the bedside of children in a diabetes camp [37], and subsequent transition to patients’ homes [34]. In 2011, we introduced the first wearable AID system – the Diabetes Assistant (DiAs) – built using an Android smart phone as a computational hub to run the AID algorithm [38,39,40]. Studies enrolling adults, adolescents, and children have shown improved glycemic control while decreasing the rates of hyperglycemia and hypoglycemia in inpatient trials [41,42], at diabetes camps [37,43,44], and in outpatient environments [45,46,47]. In September 2016, the FDA approved the first hybrid AID system – the Medtronic 670G – which is capable of automatically adjusting the pump’s basal rate, but still does not automate insulin boluses [48]. In the past 6 years, our AID studies have enrolled more than 450 patients with T1D who used our smartphone-based system (DiAs and its descendant inControl) for over 300,000 hours of use to date in the U.S. and overseas. Below we propose changes to the UVA/Padova T1D Simulator to provide an in silico description of glucose control after islet transplantation. The rationale, approach used to modify the simulator, and the results obtained from several in silico scenarios are discussed. Further, we implemented a possible AID strategy for islet recipients, which relies on the modified models.
4. Simulation Platform for Islet Transplantation
4.1 T1D Simulator Modifications
The UVA/Padova T1D Simulator introduced in [20] was modified to accommodate metabolic changes introduced by islet transplantation (T1D-IT Simulator), including: 1) describe the overall glucose/insulin metabolism after surgery; 2) represent islets secretion in the portal vein, progression and decay, and 3) design, and test in silico closed-loop algorithms to assist glycemic control. In the absence of detailed data on the influence of graft location on metabolic control, we have considered the portal vein in the liver as the “classic” site for successful islet infusion [49]. Consequently, the modification of the T1D Simulator will focus on islet transplantation in the liver via the portal vein.
Following the widely adopted Edmonton Protocol [12], the islets infused in the portal vein produce insulin responding to glucose variations. Insulin excursions to exogenous glucose intake were observed in eight islet transplant recipients after 2-12 months of their last islet infusion [50]. The insulin response was improved compared to T1D subjects, but still inferior to health. Similarly, significant impaired first-phase response to intravenous glucose and blunted response to an orally consumed meal were also found in the assessment of β–cell function after islet transplantation [51]. Thus, the modeling of insulin dynamics in islet recipients is similar to that in T2D subjects [24]. The initial modifications include insulin secretion, inhibition of endogenous glucose production, and change of insulin concentration in the liver. It has to be noted that the following modifications are for conceptual demonstration only, since the physiology of glucose metabolism after islet transplantation may be altered dramatically, and the governing equations require both careful and systematic investigation with further data.
Insulin Secretion. Insulin production of islets infused into the portal vein can be described by the following equations [24],
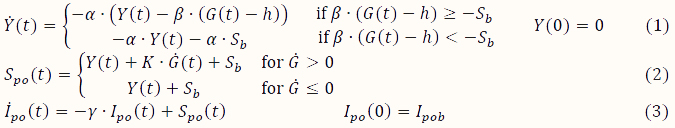
where Y(t) represents one part of insulin secretion that is stimulated by glucose concentration above a certain threshold h (set to basal glucose concentration Gb); Spo (t) represents the overall insulin secretion in the portal vein; the parameter α represents the delay of signals; β represents the insulin secretion response to glucose concentration; K represents the insulin secretion responsive ability to the rates of glucose change; γ represents the diffusion parameter of insulin between the portal vein and the liver – a process that is governed by the equation:
![]()
Thus, the insulin concentration in the liver ( ) can be determined by
) can be determined by
![]()
where I_p represents the insulin concentration in the plasma; m_1 and m_30 represent the transfer rate out of the liver and the clearance rate in the liver respectively.
Endogenous Glucose Production (EGP). As the endogenous glucose production may be inhibited by insulin in the portal vein [24], the calculation of EGP in the simulator should have an additional term ( I_po (t)) representing the impact of islets in the portal vein. The EGP is given by
![]()
where G_p is the glucose concentration in plasma; I_d is the delayed insulin signal; 〖GLG〗_d is the glucagon action; k_p1is EGP at zero glucose and insulin, k_p2 is the liver glucose effectiveness parameter, k_p3 represents the amplitude of insulin action on the liver, k_"counter" represents the amplitude of glucagon action on EGP in the liver, and k_p4 represents the amplitude of portal insulin inhibition on the liver.
4.2 Parameters Selection
In the T1D-IT Simulator, the basal state of glucose concentration (G_b) was reduced to 55% of the values adopted for the T1D in silico subjects, to represent an improved glycemic control after surgery. There are different findings on insulin resistance for using immunosuppressive drugs [52,53,54]. In the proposed simulation, a 20% decrease of insulin-dependent glucose transport (basal and maximal rates, V_m0 and V_mx) was set to represent increased insulin resistance. The other parameters proposed in the simulation are given in Table 1.
The parameters values for normal and T2D subjects reported in Table 1 are adopted from [24]. The principle of parameters selection and tuning for islet recipients is to represent the improvement of glycemic control soon after surgery.
Table 1 Parameters values.

4.3. In Silico Representation of Islet Recipients
With parameters modified for islet recipients (Table 1), we ran simulations without exogenous insulin injection on 100 adult in silico subjects with T1D. Three meals in a 24-hr day were given as [0.6, 1.3, 1.0] g carbohydrate per kg body weight at times [0700, 1200, 1800].
The daily pattern of glucose concentration is shown in Figure 2A. The deep and light red areas respectively represent the 25th-75th and 10th-90th inter-quantile ranges of glucose concentrations in the virtual subject population. At the beginning of the experiment, the fasting glucose concentrations is between 80 and 110 mg/dl. The three glucose excursions correspond to meals. With 100% islet replacement, post-absorptive glucose concentrations are well maintained, but the postprandial excursions are generally higher than those in health.
With decrease of the mass of functional islets, the ability to maintain normoglycemia is gradually lost. In silico, the level of islet mass deterioration is represented by decreasing the values of insulin secretion parameters, β and K. The simulation was repeated with different islet mass equal to 100%, 66%, 33% and 0% of full islet replacement (Figure 2). The loss of islet mass (decreased insulin secretion) elevated the fasting glucose concentration and decreased the ability of insulin secretion to control meals. An extreme case would be a total destruction of islets (Figure 2D). In this case, glucose concentration continues to climb up if no exogenous insulin is administered (Figure 2D).

Figure 2 24-hour glucose concentrations with three meals computer simulated with different islet mass. A) 100% B) 66% C) 33% D) 0%. The bold black curve represents mean glucose concentrations. The two black solid horizontal lines represent glucose concentrations at 70 mg/dl and 180 mg/dl, respectively. Glucose trend between two vertical dashed lines (before breakfast) represents elevated fasting glucose concentration as islet mass decreases. The deep and light red areas respectively represent the 25th-75th and 10th-90th inter-quantile ranges of CGM values in the virtual subject population.
While Figure 2 is only an initial illustration of the in silico modeling of islet transplantation; when fully developed, the T1D-IT Simulator can provide a framework for design, testing, and pre-clinical validation of closed-loop algorithms augmenting islet transplantation.
To achieve this objective, we need to confirm the existing, or reconfigure, the governing model equations to adapt the simulator for islet recipients. For example, in the original T1D Simulator, the feedback relationship between glucagon and insulin is weakened due to the loss of endogenous insulin [55]. This may not be the case for islets recipients because islets including α-cells, β-cells, and δ-cells are infused into the portal vein and therefore glucagon-insulin feedback mechanisms and glucagon counterregulation should be theoretically preserved, at least to a certain level. In dogs with intrahepatic islets infusion, a certain level of glucagon response was observed, but the protection against hypoglycemia was lost (Figure 3 in [56]). Similarly, in human subjects (Figure 2 in [56]). Thus, the mechanism of glucagon secretion in the portal vein and any associated hypoglycemia protection should be further investigated. This will necessitate modification of the pharmacodynamics equations and parameter re-estimation. Another candidate of modification would be GLP-1, which stimulates insulin release upon meal intake. GLP-1 is secreted in the intestine and about 25% reaches liver [57]. Normally, the signal from GLP-1 to β-cells in pancreas is indirect, while for the islet recipients, GLP-1 would act directly on islets in the portal vein. Thus, it would be important to check whether and how GLP-1 may impact insulin secretion of transplanted islets. Finally, a key step to be taken is to check which parameters of the in silico model (e.g., glucose responsiveness, insulin action, insulin resistance) change due to immunosuppression and other factors post-surgery. Thus, comprehensive data will be required to identify and validate model parameters and inter-subject parameter variation.
5. The Role of AID in Patients with T1D after Islet Transplantation
A major objective of the in silico modeling described in the previous section is the development of a versatile platform to design, test, and validate closed-loop algorithms assisting islet transplantation patients with their residual exogenous insulin needs. Although AID can be implemented by intravenous [58] or intraperitoneal [59] routes, here we discuss subcutaneous insulin delivery given its benefits and reliability in an outpatient setting.
5.1 Adapting AID for Islet Transplant Recipients
To the best of the authors’ knowledge, research on automated insulin dosing in islet transplant recipients is still incipient. Forlenza et al in [60] reported the feasibility and efficacy of closed-loop therapy (Medtronic ePID 2.0, Medtronic Diabetes, CA) in islet autotransplant recipients. In this work, fourteen adults (36% male) were randomized to closed-loop continuous subcutaneous insulin infusion (CL-CSII) or multiple daily injections (MDI) for 72 hours after transplantation. The authors reported significant improvement in the glycemic trends under CL-CSII when compared to conventional therapy during the period of islet engraftment. It should be noted, however, that in this study autotransplantation was performed, which implies that the transplant was not prompted by T1D, but by different pathology, e.g. chronic pancreatitis. Nevertheless, AID could become an appealing alternative to increase the chances for success during engraftment period because maintaining normoglycemia favors the survival of the transplanted β-cells [60]. This is particularly relevant beyond the immediate postoperative period during which intravenous continuous insulin infusion is the standard of care [61].
Building on the progress of AID in the past decade, we now formulate an approach to the design of AID for islet transplant recipients, see Figure 3. The transplanted islets produce unknown amounts of insulin and glucagon that may or may not ensure hormonal replacement. In addition, since transplanted islets are spread into the portal vein branches within the liver, phenomena like first pass hepatic insulin extraction and effect on the stimulation/inhibition of glycogenesis and glycogenolysis need to be further studied.

Figure 3 The closed-loop AID system for islet transplant recipients. EIP and EGLP stand for Endogenous Insulin Production and Endogenous Glucagon Production, respectively.
From control point of view, the AID system input remains CGM and the AID output remains the rate of subcutaneously injected insulin. However, the unknown/unmeasured disturbances now include endogenous insulin and glucagon production, in addition to meal timing, carb amount, and exercise duration and intensity. Moreover, the correct pairing of the relatively slow subcutaneous insulin absorption and the faster endogenous insulin produced by the transplanted islets becomes a major challenge. Thus, model individualization/identification will be needed to tailor the AID algorithm to individual patient’s physiology and to individual degrees of success of islet transplantation. All numerical results are obtained with a modified version of the Subcutaneous Oral Glucose Minimal Model (SOGMM) presented in [62] with the equations introduced in Section “Simulation Platform for Islet Transplantation” presented in the Appendix.
5.2. Case Study – AID for an Islet Transplant Recipient, in silico Results
Consider an adult patient with T1D (diagnosis > 20y, last HbA1c of 8.2%, BMI of 27 kg/m2, BW: 85 kg) with high blood glucose variability and hypoglycemia unawareness, who has been on CSII for more than a year. Two scenarios are presented. In the first scenario, the patient underwent an intraportal islet transplantation (~7000 IEQ/kg from a 56-y-old male with BMI of 24 kg/m2 and no history of diabetes). In the postoperative period, the patient received intravenous continuous insulin infusion therapy (PI controller) with tight glycemic outcomes [70 – 180 mg/dl]. After recovery, the patient is transitioned to AID and observed for two days. The second scenario presents a control patient who is not placed on AID, but has otherwise identical characteristics and the same operative and postoperative management. In both scenarios, the patient has the following meal schedule: 50g, 110g, and 85g CHO at 7:00 a.m ± 10 min, 1:00 p.m ± 10 min, and 7:00 p.m ± 10 min, respectively. Basal insulin is adjusted to 10 mU/min (before surgery and during AID in the experimental patient). Figure 4 shows the time sequence of the simulation experiment.

Figure 4 Time sequence of the in silico experiment.
Figure 5 shows the glucose profile for both control and experimental in silico “patients”: Before the surgery, the virtual patients exhibited high BG variability similar to brittle diabetes, despite being treated according to their recommended basal insulin profiles and insulin boluses. After surgery, the patients were started on continuous i.v. insulin infusion protocol (recovery time) to maintain blood glucose concentration in the range of 80-125 mg/dl with no oral intake (instead, patients were fed via jejunal tube). Once patients reached full enteral nutrition, i.v. insulin was discontinued and the AID system were started for the experimental patient.
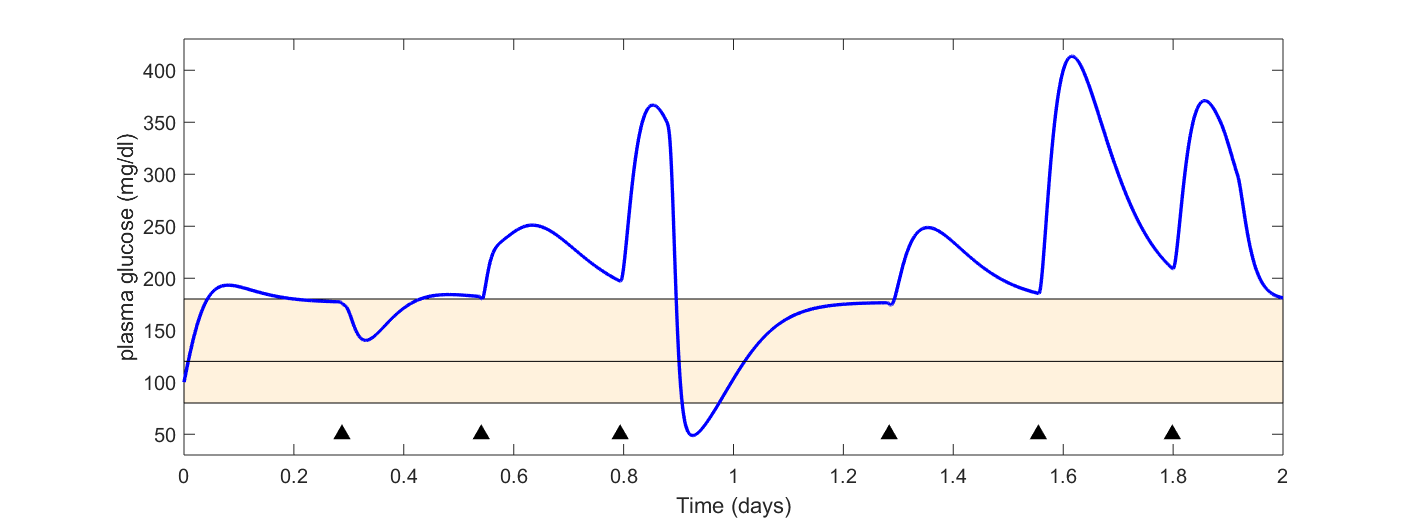
Figure 5 2-day monitoring before surgery preparation (starting at 12 a.m). Both control and experimental are assumed to have identical characteristics. The yellow area corresponds to the safe region (80-180 mg/dl). Black triangles denote the times of meal intake.
Figure 6 compares the glucose profiles of the experimental and control in silico “patients” during the two-day intervention, i.e., after recovery time. The experimental patient uses a PI controller whose parameters are presented in Table 2. In the case of the experimental patient (Gp T1D-IR C), the controller was able to maintain the glucose concentration around the set-point (120 mg/dl), although mild hypoglycemic events occur. Realistic insulin profiles were administered as seen in the figure at the bottom. Although the patients recovered partially their insulin secretion, insulin independence is not achieved and high postprandial glucose peaks appear, compromising the engraftment revascularization and favoring β-cells apoptosis [60].
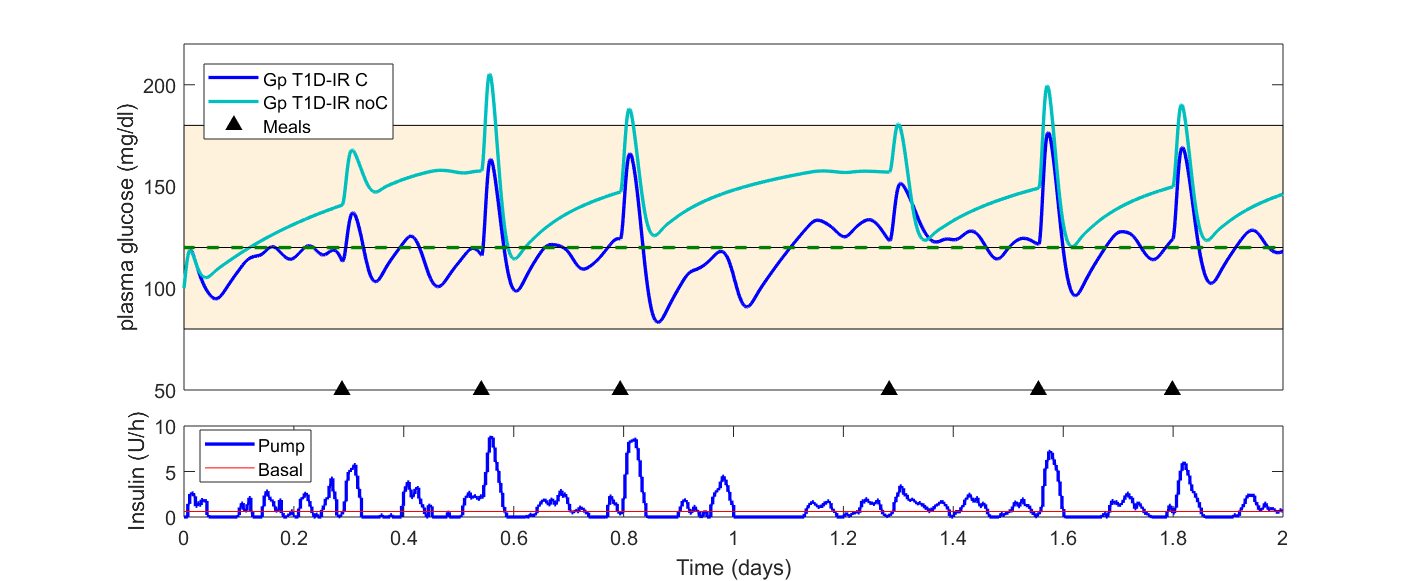
Figure 6 Comparison of the two proposed scenarios. Gp T1D-IR C stands for plasma glucose concentration during the AID intervention (experimental) and Gp T1D-IR noC stands for plasma glucose concentration with no exogenous insulin (control). The green dotted line corresponds to the set-point for the controller (120 mg/dl). The yellow area corresponds to the safe region (80-180 mg/dl).
Table 2 PI controller tuning. K_p and K_I stand for proportional and integral gains, respectively.

6. Discussion
Human islet transplantation is becoming an appealing alternative to exogenous insulin treatment in the management of T1D. While lack of islets supply still limits the applicability of this technique, significant improvement has been achieved regarding islet isolation and preparation, as well as in terms of post-transplant immunosuppression therapies.
In this manuscript, we have discussed the possibility of integrating the transplant procedure with a post-transplant AID system designed to compensate for residual insulin needs transplanted patients may experience. To accomplish this, we have proposed modelling approaches able to integrate the current knowledge about glucose-insulin regulation in T1D, with the partially restored endogenous insulin secretion that islet recipients would benefit from. By resorting to the UVA/Padova T1D Simulator, we used a population of 100 in silico subjects to simulate the postprandial control of islet recipients at different stages after the transplant procedure, and we further discussed a possible AID strategy that could be deployed to support transplanted individuals. Our aim is to demonstrate that safe and reliable automated insulin infusion systems may help maintaining normoglycemia after islet transplantation, thus favoring the engraftment revascularization, decreasing the glycemic stress transplanted islets are exposed to, and potentially extending the life of the graft.
Limitations of the proposed approach are linked to the need for T1D patients who decide to choose it as a treatment strategy, to undergo a minimally-invasive surgical procedure followed by a lifetime of immunosuppression therapy and simultaneous exogenous insulin administration by a potentially cumbersome AID system, which relies on the use of CGM and CSII devices. Accurate CGM systems are needed to optimize AID performance, and this oftentimes requires the patient to calibrate the device once or twice daily, which can be bothersome to patients who already underwent a surgical procedure to stabilize the control of their diabetes. On the other hand, islet transplantation is devised for patients with unstable T1D who cannot be successfully stabilized with insulin pump and/or CGM therapies, and long-term post-transplant insulin-independence seems to be difficult to achieve. Combining islet transplantation and post-transplant insulin therapy appears therefore necessary, and in this scenario, treatment based on AID may represent the optimal solution to minimize the glycemic stress transplanted islets are exposed to and extend the life of the graft. How palatable is this combined approach to patients remains an open question that will need to be addressed.
Future work will be devoted to test and validate our T1D-IT Simulator with clinical data from islet recipients. Glucose, insulin, and C-peptide time series collected during various tests (e.g., intravenous or glucose tolerance test) would represent valuable datasets to allow a more precise, data-driven modeling of glucose homeostasis after islet transplantation. Model parameters could be estimated on available data, and subsequently used to create a population of in silico transplanted subjects, potentially deployable to test and optimize control strategies. This population would be representative of the inter-subject variability expected following islet transplantation, that we could not describe in our simulation (insulin secretion parameters were given as population values) due to the limited availability of data.
We believe that integrating the transplant procedure with post-transplant AID systems could reduce the number of islets to be transplanted, thus mitigating the current problem of limited islet supply and potentially reducing the need for potent immunosuppression. If further studies confirm these speculations, the combination of islet transplantation and AID therapy could represent a breakthrough in the treatment of diabetes.
Acknowledgments
We would like to thank Professor Kenneth Brayman for the kind invitation to contribute to this project, Professor Boris Kovatchev for the opportunity of writing the manuscript, and his guidance and supervision throughout the entire process, and Professor Marc Breton for support and discussions.
Author Contributions
DL, JCT, and CF equally contributed to the design and implementation of the study, and to the writing of the manuscript.
Funding
This work has been supported by the University of Virginia Strategic Investment Fund for Type 1 Diabetes research.
Competing Interests
The authors have declared that no competing interests exist.
Appendix: Mathematical Model for AID Design
For the design and testing of the AID system, we used an extended version of the Subcutaneous Oral Glucose Minimal Model (SOGMM) presented in [62] with the equations presented in Section “Simulation Platform for Islet Transplantation”.
Before islet transplantation
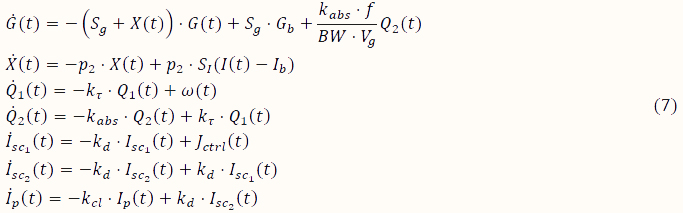
with
![]()
After islet transplantation:
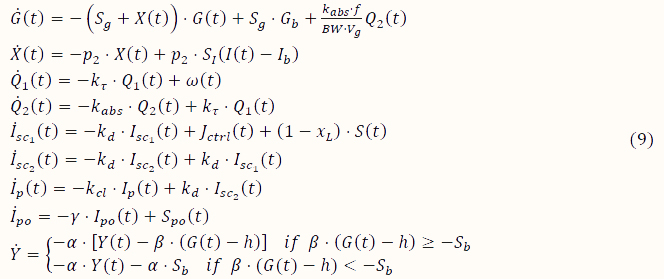
with
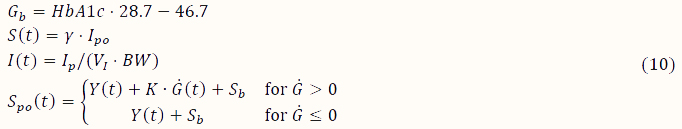
where G (mg/dl) is the plasma glucose concentration, X (1/min) the proportion of insulin in the remote compartment, Q_1 (mg) the glucose mass in the stomach, Q_2 (mg) glucose mass in the gut, 〖I_sc〗_1 (mU) and 〖I_sc〗_2 (mU) the insulin amount in the first and second compartment, respectively, I_p (mU) the plasma insulin, I_po (mU) the insulin in the portal vein, Y (mU) the part of insulin secretion stimulated by glucose concentration above basal glucose (G_b), S_po (t) (mU) the overall insulin secretion in the portal vein, S(t) (mU) secreted insulin diffused into the liver, ω (mg/min) the rate of mixed-meal carbohydrate absorption, and J_ctrl (mU/min) the exogenous insulin. The parameters of (7-10) are presented in Table A1. Basal glucose is computed as indicated in [62].
Table A1 Model Parameters with population values for (7) - (10).

References
- Cobelli C, Dalla Man C, Sparacino G, Magni L, De Nicolao G, Kovatchev BP. Diabetes: models, signals, and control. IEEE Rev Biomed Eng. 2009; 2: 54. [CrossRef]
- Group DR. The Diabetes Control and Complications Trial (DCCT): design and methodologic considerations for the feasibility phase. Diabetes. 1986; 35: 530-545. [CrossRef]
- Control D, Group CTR. The relationship of glycemic exposure (HbA1c) to the risk of development and progression of retinopathy in the diabetes control and complications trial. Diabetes. 1995; 44: 968-983. [CrossRef]
- Cryer P. Hypoglycaemia: the limiting factor in the glycaemic management of type I and type II diabetes. Diabetologia. 2002; 45: 937-948. [CrossRef]
- Hovorka R. Closed-loop insulin delivery: from bench to clinical practice. Nat Rev Endocrinol. 2011; 7: 385. [CrossRef]
- Renard E, Cobelli C, Zisser HC, Kovatchev BP. Artificial pancreas goes outpatient: a new diabetes ecosystem. J Diabetes Sci Technol. 2013; 7: 1411-1415. [CrossRef]
- Cobelli C, Renard E, Kovatchev B. Artificial pancreas: past, present, future. Diabetes. 2011; 60: 2672-2682. [CrossRef]
- Cefalu WT, Tamborlane WV. The artificial pancreas: are we there yet? Diabetes Care. 2014; 37: 1182-1183. [CrossRef]
- Kudva YC, Carter RE, Cobelli C, Basu R, Basu A. Closed-loop artificial pancreas systems: physiological input to enhance next-generation devices. Diabetes care. 2014; 37: 1184-1190. [CrossRef]
- Kovatchev B. The artificial pancreas in 2017: The year of transition from research to clinical practice. Nat Rev Endocrinol. 2017; 14: 74. [CrossRef]
- Shapiro AJ, Pokrywczynska M, Ricordi C. Clinical pancreatic islet transplantation. Nat Rev Endocrinol. 2017; 13: 268. [CrossRef]
- Shapiro AJ, Lakey JR, Ryan EA, Korbutt GS, Toth E, Warnock GL, et al. Islet transplantation in seven patients with type 1 diabetes mellitus using a glucocorticoid-free immunosuppressive regimen. N Eng J Med. 2000; 343: 230-238. [CrossRef]
- Ryan EA, Paty BW, Senior PA, Bigam D, Alfadhli E, Kneteman NM, et al. Five-year follow-up after clinical islet transplantation. Diabetes. 2005; 54: 2060-2069. [CrossRef]
- Shapiro AJ, Ricordi C, Hering BJ, Auchincloss H, Lindblad R, Robertson RP, et al. International trial of the Edmonton protocol for islet transplantation. N Eng J Med. 2006; 355: 1318-1330. [CrossRef]
- Berney T, Ferrari‐Lacraz S, Bühler L, Oberholzer J, Marangon N, Philippe J, et al. Long‐term insulin‐independence after allogeneic islet transplantation for type 1 diabetes: over the 10‐year mark. Am J Transplant. 2009; 9: 419-423. [CrossRef]
- Lakey JR, Burridge PW, Shapiro AJ. Technical aspects of islet preparation and transplantation. Transpl Int. 2003; 16: 613-632. [CrossRef]
- Shapiro AJ. State of the art of clinical islet transplantation and novel protocols of immunosuppression. Curr Diab Rep. 2011; 11: 345. [CrossRef]
- Bellin MD, Barton FB, Heitman A, Harmon J, Kandaswamy R, Balamurugan A, et al. Potent induction immunotherapy promotes long‐term insulin independence after islet transplantation in type 1 diabetes. Am J Transplant. 2012; 12: 1576-1583. [CrossRef]
- Kovatchev BP, Breton M, Dalla Man C, Cobelli C. In silico preclinical trials: a proof of concept in closed-loop control of type 1 diabetes. J Diabetes Sci Technol. 2009; 3: 44-55. [CrossRef]
- Man CD, Micheletto F, Lv D, Breton M, Kovatchev B, Cobelli C. The UVA/PADOVA type 1 diabetes simulator: new features. J Diabetes Sci Technol. 2014; 8: 26-34. [CrossRef]
- Visentin R, Campos-Náñez E, Schiavon M, Lv D, Vettoretti M, Breton M, et al. The UVA/Padova Type 1 Diabetes Simulator Goes From Single Meal to Single Day. J Diabetes Sci Technol. 2018; 12: 273-281. [CrossRef]
- Kovatchev B, Breton M, Dalla Man C, Cobelli C. In silico model and computer simulation environment approximating the human glucose/insulin utilization. Master File MAF-1521. Food and Drug Administration (FDA), Silver Spring, MA. 2008.
- Viceconti M, Cobelli C, Haddad T, Himes A, Kovatchev B, Palmer M. In silico assessment of biomedical products: the conundrum of rare but not so rare events in two case studies. Proc Inst Mech Eng H. 2017; 231: 455-466. [CrossRef]
- Dalla Man C, Rizza RA, Cobelli C. Meal simulation model of the glucose-insulin system. IEEE Trans Biomed Eng. 2007; 54: 1740-1749. [CrossRef]
- Wang Q, Liang X, Wang S. Intra-islet glucagon secretion and action in the regulation of glucose homeostasis. Front Physiol. 2013; 3: 485. [CrossRef]
- Cryer PE. Minireview: Glucagon in the pathogenesis of hypoglycemia and hyperglycemia in diabetes. Endocrinology. 2012; 153: 1039-1048. [CrossRef]
- Cryer PE. Mechanisms of hypoglycemia-associated autonomic failure in diabetes. New Eng J Med. 2013; 369: 362-372. [CrossRef]
- Cobelli C, Dalla Man C, Toffolo G, Basu R, Vella A, Rizza R. The oral minimal model method. Diabetes. 2014; 63: 1203-1213. [CrossRef]
- Bergman RN, Ider YZ, Bowden CR, Cobelli C. Quantitative estimation of insulin sensitivity. Am J Physiol. 1979; 236: E667.
- Kovatchev B, Tamborlane WV, Cefalu WT, Cobelli C. The artificial pancreas in 2016: a digital treatment ecosystem for diabetes. Diabetes Care. 2016; 39: 1123-1126. [CrossRef]
- Thabit H, Hovorka R. Coming of age: the artificial pancreas for type 1 diabetes. Diabetologia. 2016; 59: 1795-1805. [CrossRef]
- Doyle FJ, Huyett LM, Lee JB, Zisser HC, Dassau E. Closed-loop artificial pancreas systems: engineering the algorithms. Diabetes care. 2014; 37: 1191-1197. [CrossRef]
- Steil GM, Rebrin K, Darwin C, Hariri F, Saad MF. Feasibility of automating insulin delivery for the treatment of type 1 diabetes. Diabetes. 2006; 55: 3344-3350. [CrossRef]
- Anderson SM, Raghinaru D, Pinsker JE, Boscari F, Renard E, Buckingham BA, et al. Multinational home use of closed-loop control is safe and effective. Diabetes Care. 2016: dc152468. [CrossRef]
- Bekiari E, Kitsios K, Thabit H, Tauschmann M, Athanasiadou E, Karagiannis T, et al. Artificial pancreas treatment for outpatients with type 1 diabetes: systematic review and meta-analysis. BMJ. 2018; 361: k1310. [CrossRef]
- Weisman A, Bai J-W, Cardinez M, Kramer CK, Perkins BA. Effect of artificial pancreas systems on glycaemic control in patients with type 1 diabetes: a systematic review and meta-analysis of outpatient randomised controlled trials. Lancet Diabetes Endocrinol. 2017; 5: 501-512. [CrossRef]
- Phillip M, Battelino T, Atlas E, Kordonouri O, Bratina N, Miller S, et al. Nocturnal glucose control with an artificial pancreas at a diabetes camp. N Engl J Med. 2013; 368: 824-833. [CrossRef]
- Keith-Hynes P, Guerlain S, Mize B, Hughes-Karvetski C, Khan M, McElwee-Malloy M, et al. DiAs user interface: a patient-centric interface for mobile artificial pancreas systems. J Diabetes Sci Technol. 2013; 7: 1416-1426. [CrossRef]
- Place J, Robert A, Ben Brahim N, Keith-Hynes P, Farret A, Pelletier M-J, et al. DiAs web monitoring: a real-time remote monitoring system designed for artificial pancreas outpatient trials. J Diabetes Sci Technol. 2013; 7: 1427-1435. [CrossRef]
- Keith-Hynes P, Mize B, Robert A, Place J. The Diabetes Assistant: a smartphone-based system for real-time control of blood glucose. Electronics. 2014; 3: 609-623. [CrossRef]
- Weinzimer SA, Steil GM, Swan KL, Dziura J, Kurtz N, Tamborlane WV. Fully automated closed-loop insulin delivery versus semiautomated hybrid control in pediatric patients with type 1 diabetes using an artificial pancreas. Diabetes Care. 2008; 31: 934-939. [CrossRef]
- Elleri D, Allen JM, Nodale M, Wilinska ME, Mangat JS, Larsen AMF, et al. Automated overnight closed-loop glucose control in young children with type 1 diabetes. Diabetes Technol Ther. 2011; 13: 419-424. [CrossRef]
- Russell SJ, El-Khatib FH, Sinha M, Magyar KL, McKeon K, Goergen LG, et al. Outpatient glycemic control with a bionic pancreas in type 1 diabetes. N Eng J Med. 2014; 371: 313-325. [CrossRef]
- Ly TT, Breton MD, Keith-Hynes P, De Salvo D, Clinton P, Benassi K, et al. Overnight glucose control with an automated, unified safety system in children and adolescents with type 1 diabetes at diabetes camp. Diabetes Care. 2014; 37: 2310-2316. [CrossRef]
- Thabit H, Tauschmann M, Allen JM, Leelarathna L, Hartnell S, Wilinska ME, et al. Home use of an artificial beta cell in type 1 diabetes. N Engl J Med. 2015; 373: 2129-2140. [CrossRef]
- Kovatchev BP, Renard E, Cobelli C, Zisser HC, Keith-Hynes P, Anderson SM, et al. Safety of outpatient closed-loop control: first randomized crossover trials of a wearable artificial pancreas. Diabetes care. 2014; 37: 1789-1796. [CrossRef]
- Breton MD, Cherñavvsky DR, Forlenza GP, DeBoer MD, Robic J, Wadwa RP, et al. Closed loop control during intense prolonged outdoor exercise in adolescents with type 1 diabetes: the artificial pancreas ski study. Diabetes Care. 2017; 40: 1644-1650. [CrossRef]
- Bergenstal RM, Garg S, Weinzimer SA, Buckingham BA, Bode BW, Tamborlane WV, et al. Safety of a hybrid closed-loop insulin delivery system in patients with type 1 diabetes. JAMA. 2016; 316: 1407-1408. [CrossRef]
- Cantarelli E, Piemonti L. Alternative transplantation sites for pancreatic islet grafts. Curr Diab Rep. 2011; 11: 364-374. [CrossRef]
- Rickels MR, Naji A, Teff KL. Insulin sensitivity, glucose effectiveness, and free fatty acid dynamics after human islet transplantation for type 1 diabetes. J Clin Endocrinol Metab. 2006; 91: 2138-2144. [CrossRef]
- Rickels MR, Schutta MH, Markmann JF, Barker CF, Naji A, Teff KL. β-Cell function following human islet transplantation for type 1 diabetes. Diabetes. 2005; 54: 100-106. [CrossRef]
- Froud T, Ricordi C, Baidal DA, Hafiz MM, Ponte G, Cure P, et al. Islet transplantation in type 1 diabetes mellitus using cultured islets and steroid‐free immunosuppression: Miami experience. Am J Transplant. 2005; 5: 2037-2046. [CrossRef]
- Fernandez LA, Lehmann R, Luzi L, Battezzati A, Angelico MC, Ricordi C, et al. The Effects Of Maintenance Doses Of Fk506 Versus Cyclosporin A On Glucose And Lipid Metabolism After Orthotopic Liver Transplantation1. Transplantation. 1999; 68: 1532-1541. [CrossRef]
- Rickels MR, Kong SM, Fuller C, Dalton-Bakes C, Ferguson JF, Reilly MP, et al. Improvement in insulin sensitivity after human islet transplantation for type 1 diabetes. J Clin Endocrinol Metab. 2013; 98: E1780-E1785. [CrossRef]
- Farhy LS, McCall AL. Pancreatic network control of glucagon secretion and counterregulation. Methods Enzymol. 2009; 467: 547-581. [CrossRef]
- Robertson RP. Islet transplantation as a treatment for diabetes—a work in progress. N Engl J Med. 2004; 350: 694-705. [CrossRef]
- Holst JJ. The physiology of glucagon-like peptide 1. Physiol Rev. 2007; 87: 1409-1439. [CrossRef]
- Yatabe T, Nakamura R, Kitagawa H, Munekage M, Hanazaki K. A case of perioperative glucose control by using an artificial pancreas in a patient with glycogen storage disease. J Artif Organs. 2016; 19: 100-103. [CrossRef]
- Dassau E, Renard E, Place J, Farret A, Pelletier MJ, Lee J, et al. Intraperitoneal insulin delivery provides superior glycaemic regulation to subcutaneous insulin delivery in model predictive control‐based fully‐automated artificial pancreas in patients with type 1 diabetes: a pilot study. Diabetes, Diabetes Obes Metab. 2017; 19: 1698-1705. [CrossRef]
- Forlenza GP, Nathan BM, Moran AM, Dunn TB, Beilman GJ, Pruett TL, et al. Successful application of closed‐loop artificial pancreas therapy after islet autotransplantation. American Am J Transplant. 2016; 16: 527-534. [CrossRef]
- Forlenza GP, Chinnakotla S, Schwarzenberg SJ, Cook M, Radosevich DM, Manchester C, et al. Near-euglycemia can be achieved safely in pediatric total pancreatectomy islet autotransplant recipients using an adapted intravenous insulin infusion protocol. Diabetes Technol Ther. 2014; 16: 706-713. [CrossRef]
- Patek SD, Lv D, Ortiz EA, Hughes-Karvetski C, Kulkarni S, Zhang Q, et al. Empirical representation of blood glucose variability in a compartmental model. Prediction Methods for Blood Glucose Concentration: Springer; 2016. p. 133-157. [CrossRef]










